Once we pass the age of fifty, it is pretty common to experience two or more health conditions simultaneously. Disease comorbidity can really muddy the waters of healthcare and selfcare. Pelvic organ prolapse (POP) alone can create diverse physical, emotional, social, sexual, fitness, and employment difficulties to navigate. Women with pelvic organ prolapse plus additional vaginal or pelvic health issues struggle even more with magnified confusion and frustration when co-existing conditions impact their intimate zone and their intimate lives.
Tissues bulging out of the vagina, chronic constipation, and incontinence are not exactly a delight to experience once, must less navigate daily. POP typically invades women’s lives for months, sometimes years. For most women embedded in the experience, it can feel like a lifetime. When co-existing health conditions increase POP symptoms, frustration, angst, anger, and sometimes depression compound as well. One of those co-existing conditions is a chronic, inflammatory, rarely known ahead-of-the-curve skin condition called lichen sclerosus (LS).
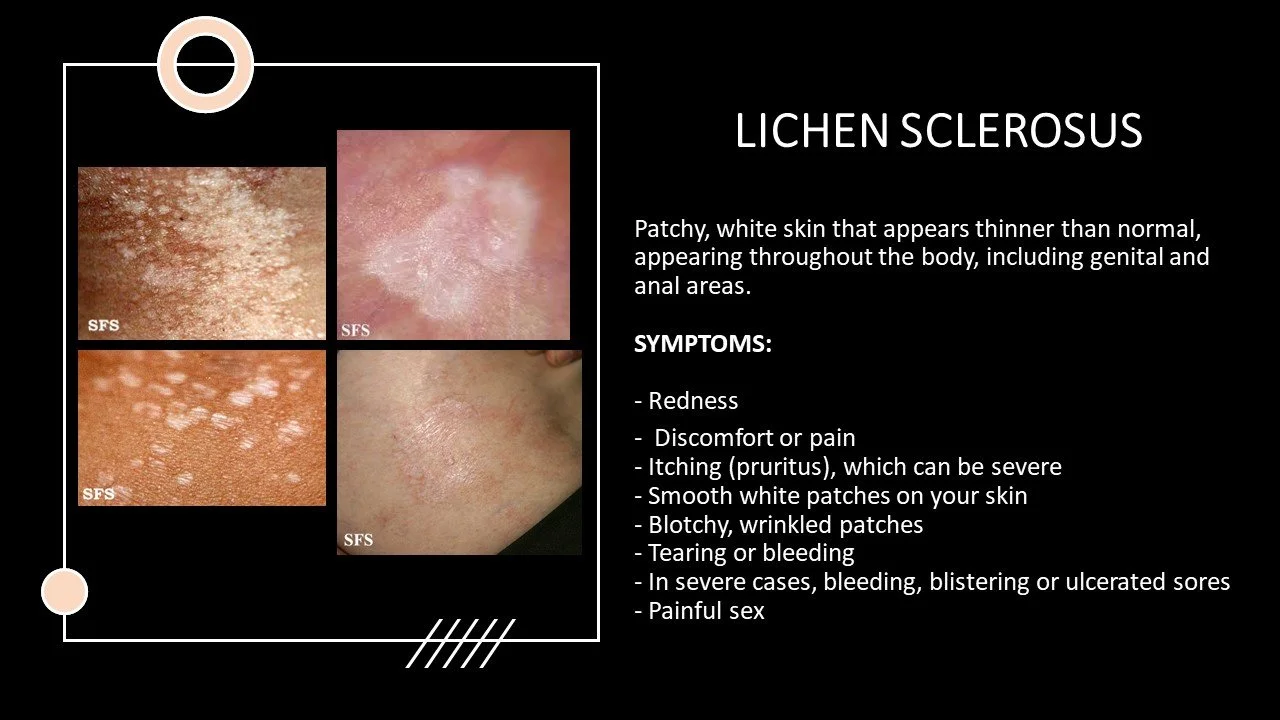
While LS can impact members of either sex at any age, it is most prevalent in females over fifty, and is estimated to impact 1 in 80 women. LS lesions usually begin as small, pink, or white bumps on the skin. Over time the rash-like area transforms into wrinkly, patchy, white patches of skin with tissue paper like consistency. The LS patches are delicate in nature, and tend to be itchy, burning, and painful, and are prone to bleeding if scratched or rubbed. With time, LS can lead to tightening and scarring of the skin, particularly around the genitals and anus. In some cases, lichen sclerosus can also lead to vulvar cancer. To add to the nightmare, LS can make sexual intercourse painful or difficult, and can understandably increase emotional reaction.
So what happens when POP and LS collide?
To expand understanding of these co-existing conditions, let’s explore LS through the mindset of lichen sclerosis expert cosmetic gynecologist Ajakaida Renaud, well versed in LS treatment protocol. Dr. Renaud is a Functional and Aesthetic Regenerative Gynecologist practicing in Venezuela. Dr. Renaud, please share a few insights about LS to clarify the backdrop.
Can you give an example of your most typical LS patient, how they are first diagnosed, how they find their way to you for treatment?
Pelvic organ prolapse is a silent and progressive pathology that can affect any woman throughout her life, exacerbated by different factors, such as overweight, pregnancy, multiparity, traumatic births (forceps delivery or long 2nd-stage labor), or hard foot-strike and heavy lifting fitness activities. POP could have a strong relationship with vulvar dermatopathies such as genital atrophic lichen sclerosus, which we well know is underestimated, since the literature tells us of 1 in 30 women in two main age groups (prepubertal and menopausal) experience LS. But we also recognize LS can manifest at any age.
What causes LS?
Occupation and most notably, aging. The loss of collagen and elasticity of the urogenital tissues leads to the triggering of this type of pathology or dysfunction of the pelvic floor, which is associated with urogenital atrophy, whether triggered postpartum, post-cancer treatment, or simply due to menopause.
Is LS contagious?
It is not contagious.
Is LS curable or must it be managed life-long?
The main objective is the early diagnosis of the disease for good management. By managing LS from the functional gynecologic and psycho-neuroimmunoendocrinology angles, we can adapt the multiple therapies that exist today on the market, according to the individual patient’s needs. In order to maintain extended periods of remission, the patient must always follow through with at least one health examination per year after discharge post-diagnosis.
What does your most common LS treatment consist of or is it different for every patient?
Each patient is different. However the basics begin with functional management, including diet low in gluten and sugars and many vegetables to improve the intestinal and endocrine axis, and thus the intestinal microbiota so that the vaginal microbiota can improve and be stable. We recommend different supplements or nutraceuticals, and we always start with platelet growth factors or PRP (at least six sessions with intervals of twenty-one days). We include red-light therapy, and massages with ozone oil in the entire periclitoral zone, corpora cavernosa, and introitus. We are currently adding exosomes as well as fractional laser and 308nm excimer laser, which acts as high-range phototherapy which has a good response to debride adhesions and increase drug delivery. We explain that it is critical to go to all consultations in a consistent manner. Following this regimen is pivotal to restore that lost collagen! We additionally add electromagnetism to all, via Hifem therapy, since a substantial percentage of these patients have associated vaginismus. Sometimes focused shock waves work effectively in the vulvar region and introitus as well.
Patients with pelvic organ prolapse suffer with multiple symptoms that are related to displaced organs and tissues. Those experiencing a simultaneous manifestation of lichen schlerosus have a larger burden to bear, given the discomfort that manifests with this frustrating condition. Physicians managing patients with vulvar LS would be well-advised to examine patients for pelvic organ prolapse to assure the comorbidity is not occurring, compounding discomfort.
**Dr. Renaud founded and runs the LS non-profit foundation FUNDAREN, The Ajakaida Renaud Foundation for Women, working in Venezuela in two main states, Caracas and Barquisimeto, as well as Santo Domingo Dominican Republic, where around twenty patients are treated weekly in different pathologies. Treatments are provided without cost or payment.**