Although progress has occurred regarding comprehensive and coordinated women’s healthcare, a significant practice gap remains.
As women, our collective health depends on our willingness to talk openly and comfortably about vaginal health with our healthcare practitioners, but also among ourselves as a female culture. The evolution of women’s communal health rests heavily on what we are comfortable sharing with our mothers, daughters, sisters, friends, and of course our intimate partners. Social acceptance is a marker of women’s health empowerment. Somehow vaginal health remains the pariah in women’s wellness.
Multiple conditions throughout the history of women’s health have had to overcome the stigma of sexual connotation to enable open public dialogue, such as breast health and reproductive rights. The biggest barriers we have yet to conquer are related to vaginal health in general, and pelvic organ prolapse (POP) specific. Two of the most life-altering events women experience, childbirth and menopause, are the leading causes for the pandemic prevalence of POP, routinely estimated in research to impact up to 50% of women. Yet women are rarely informed of POP ahead of the curve. Discovery upon diagnosis is the status quo regarding this common, cryptic women’s health pandemic.
While medically documented dating back to the Kahun Gynecological Papyrus circa 1835 B.C.E., we have yet to break down the POP wall of silence because talking openly about tissues bulging out of the vagina is not yet acceptable within the health frame. We still view the vagina for the most part as a private, sexual space despite it being the vessel of life as well as the coupler of loving relationships.
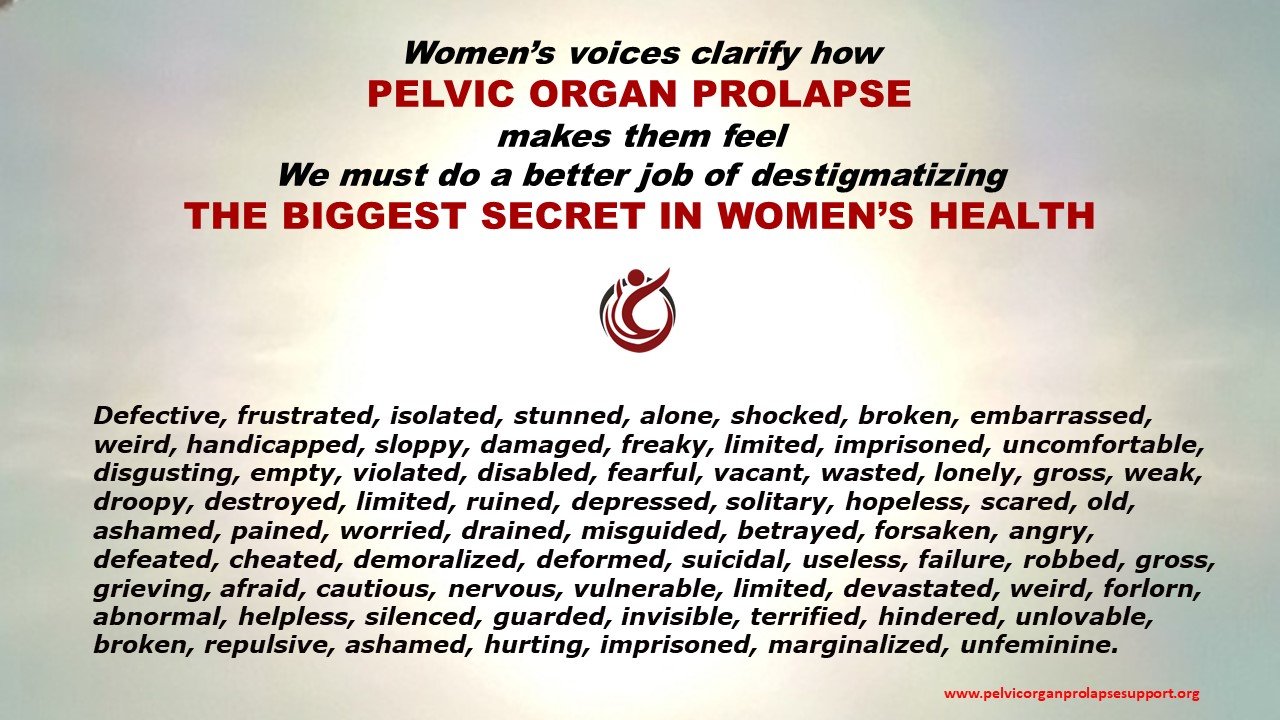
We live in a society that worships comparative perfection. While the opinions of others are irrelevant in the big picture, self-image is a significant marker of self-confidence. The plethora of hair, face, and body cosmetic items available clarifies our need for body perfection, and marketing campaigns are skilled at encouraging artful deception on the outside. How we really feel about how we look digs a bit deeper. The reality is women all too often suffer in silence with vaginal health issues that impact self-image yet remain hidden behind a wall of silence.
Shouldn't we talk about ALL women's health concerns out loud? Form, feel, function, and personal perception of the vagina and vulva are critical for optimization of vaginal and intimate health sense of self. Behind blissful birthing stories exists a cryptic aftermath that seldom makes it into the public forum. Vaginal tissue bulge, stretched vaginal gap, coital incontinence, and pain with intimacy are very common after-effects of vaginal childbirth, and very real to the women experiencing them. At times, horrific birthing experiences result in ravaged vaginal, rectal, and perineal tissue that leave women with pain and dysfunction for years, sometimes the rest of their lives, because they do not know where to go to address health concerns few talk about out loud.
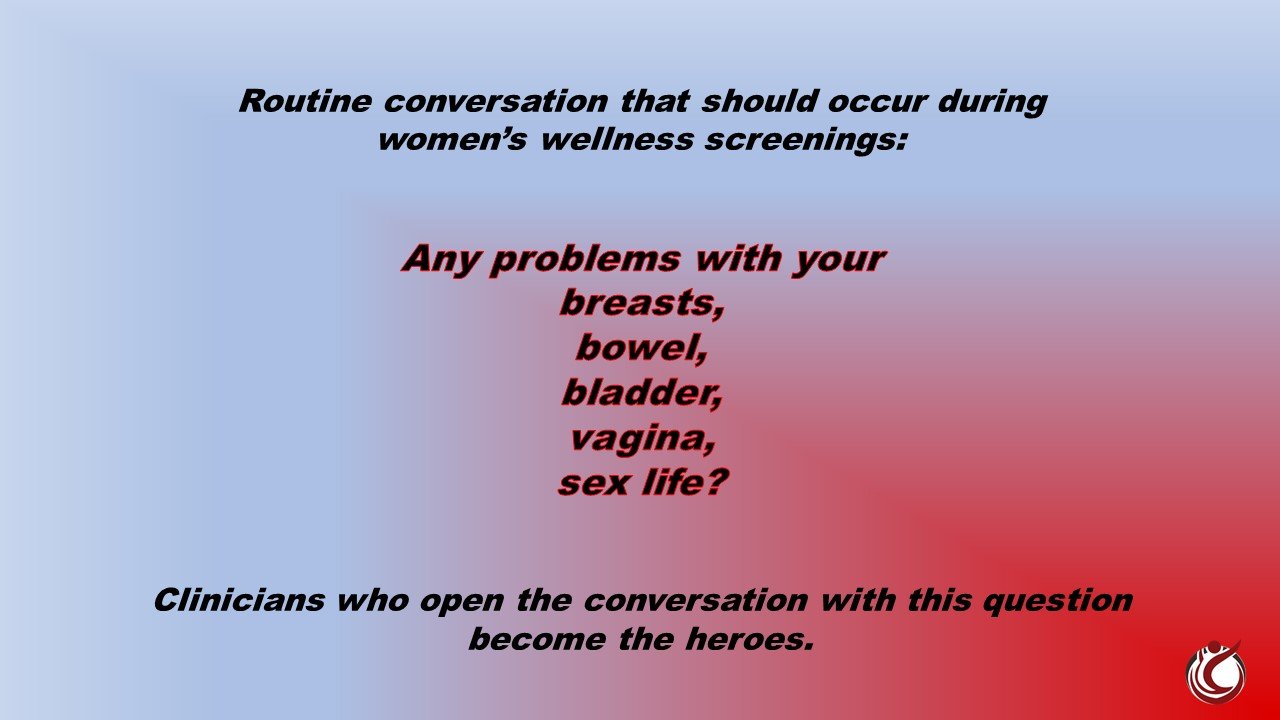
Although progress has occurred regarding comprehensive and coordinated women’s wellness screening, a significant awareness gap still exists regarding vaginal health. I ponder what the secret sauce is to destigmatize and enable all women to talk aloud comfortably about the physical, emotional, social, sexual, fitness, and employment quality of life impacts of pelvic organ prolapse. The complexity of POP necessitates a comprehensive approach to evolve women’s wellness screening, along with a multidisciplinary approach to springboard early detection and treatment.
During the breast cancer awareness transition in the 20th century prior to which breast health remained a highly stigmatized, unspoken health issue, women in positions of celebrity or political power stepped forward, associating themselves with breast health concerns. Because a few brave women in positions of influence were willing to share their stories, breast health awareness advanced and eradicated the shrouding stigma of what had been previously viewed as off the table erogenous dialogue.
~The courageous efforts of breast cancer advocate Terese Lasser, Founder of Reach to Recovery.
~The first breast cancer support initiative, Seventeen magazine editor Babette Rosmond, author of The Invisible Worm, challenging assumptions of surgeons treating women with breast cancer.
~Actress Shirley Temple Black sharing her story in McCall’s magazine.
~Former First Lady Betty Ford and Happy Rockefeller, wife of Vice-President Nelson Rockefeller, sharing their diagnoses via televised press conferences.
~NBC news correspondent Betty Rollin writing First You Cry about her experiences.
Each of these brave women increased media exposure engendering a new era in women’s breast health empowerment. We need highly prominent women in positions of visibility and voice to do the same regarding pelvic organ prolapse, ushering in the next significant revolution in women’s health empowerment.
"Open and comfortable acknowledgment of vaginal and intimate healthcare is one of the continuning challenges women face in on-going efforts to attain equal rights for our gender."
Sherrie Palm
We must disrupt women’s healthcare due process. While we certainly should celebrate the advances and changing societal perceptions in women’s health that have occurred in prior generations, it is imperative we remain cognizant and at times critical of stagnation.
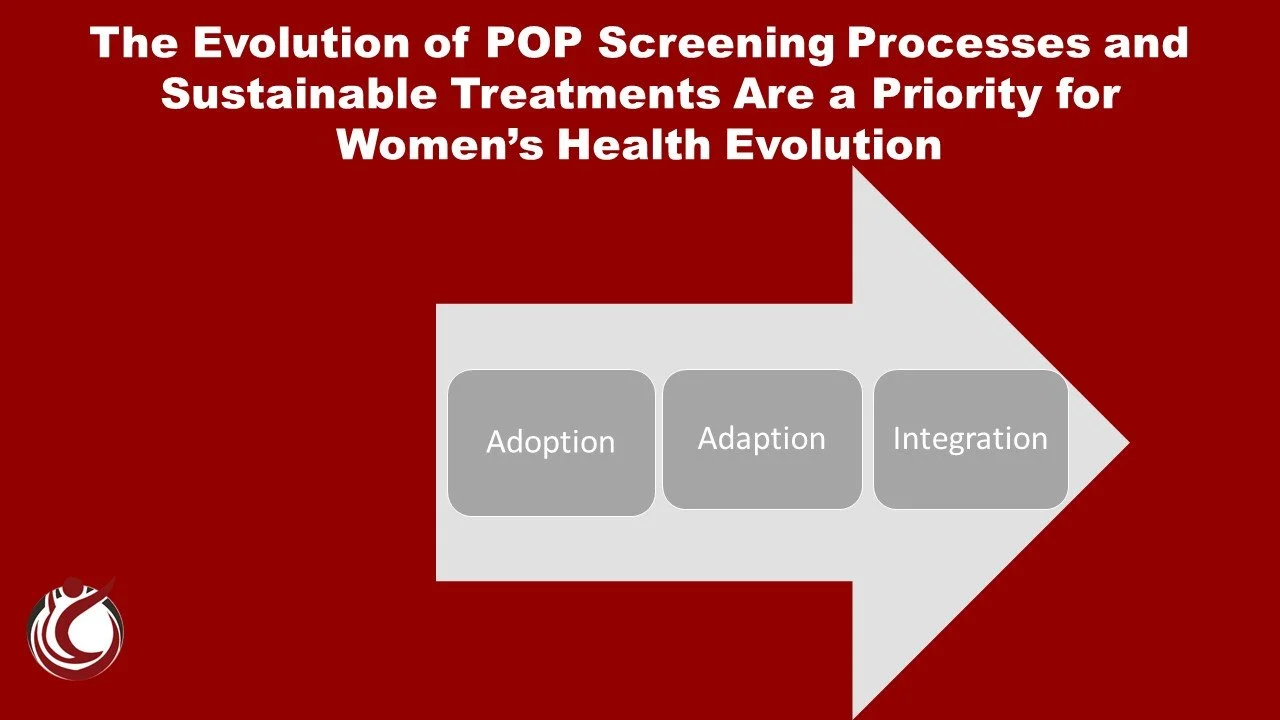
Healthcare should include delivery models shaped by female experience. But if women are not talking openly about these experiences, and healthcare does not recognize or acknowledge pandemic needs, how can we break down the barriers? Gaps in medical curriculum create roadblocks to delivery of much-needed services. FemTech dialogue looms large these days, but typically addresses fertility, menstrual, menopausal, and sexual health, rarely acknowledging the POP pandemic.
Healthcare should be accessible, preventative, proactive, and evidence based. Evolving care models create potential to overcome the current shortfall in the remaining stigmatized vaginal health care zone. It is imperative we ensure that medical disciplines of all specialties addressing basic women’s wellness are prepared to provide baseline POP screening to address needs as women flow through life transitions.
When women’s shrouded health conditions are of pandemic prevalence as is the case for POP, we must make every effort to tear down the last walls of stigmatized silence preventing women access to care. The individual threads of the fabric of women’s health policy must remain strong, but flexible and forward-thinking.
When will we reach the comfort zone with pelvic organ prolapse? Until the world at large effectively talks comfortably about this common women's health issue, little forward momentum in vaginal health empowerment will occur.
Policymakers, clinical leaders, visionary entrepreneurs, and investors each have a role to play to close gaps and overcome barriers in vaginal and intimate wellness which remain highly stigmatized. Patient voice has a significant role to play as well. All sectors engaged in the POP arena should encourage open dialogue to break down barriers and fuel the revolution in vaginal health.
The power of community will override the silence. The resilience of women openly sharing information about vaginal health will bring it to the forefront as it did breast health. Advocates, health systems, governments, and most importantly women must publicly acknowledge stigmatized health conditions to affect change.
~When we ignore the nearly 4000 years of medical documentation referencing pelvic organ prolapse, we dismiss women’s health empowerment.
~When we talk about incontinence jokingly and simply slap a pad on it as though it is not a big deal, we dismiss women’s health empowerment.
~When we block efforts to talk out loud about vaginal and intimate health in a respectful way, we dismiss women’s health empowerment.
And when we as women choose to not engage in the POP conversation openly and comfortably, we disparage the efforts of so many of our fore sisters before us who worked incredibly hard for the evolution of women’s wellness and best practice.
#APOPS #womenshealthempowerment #EveryVoiceMatters #pelvicorganprolapse
SHERRIE PALM BIO
Sherrie Palm is the Founder/CEO of Association for Pelvic Organ Prolapse Support (APOPS), a pelvic organ prolapse KOL, a global women's pelvic health advocate, a vaginal and intimate health activist, author of three editions of the award-winning book Pelvic Organ Prolapse: The Silent Epidemic and is a national and international speaker on multiple aspects of pelvic organ prolapse quality of life impact.
Sherrie’s points of focus are generating global POP awareness, developing guidance and support structures for women navigating POP, and bridge building within POP healthcare, research, academic, industry, and policy sectors toward the evolution of POP directives.
Additional information about APOPS, pelvic organ prolapse, or Sher’s book or speaking presentations is available on the APOPS website.