Enterocele, Rectocele, or Both?
Little talked about, often overlooked; enterocele is like the distant cousin who is a bit misunderstood compared to common cystocele and rectocele. Articles about pelvic organ prolapse can bevague when it comes to enterocele; this POP is sometimes undiagnosed or misdiagnosed when other types of POP are recognized (that was my scenario; a large enterocele was discovered during surgery). Let’s shine a bit of light on the difference between rectocele, intussusception, rectal prolapse, and enterocele.
A rectocele is a bulge in the anterior (front) or posterior (rear) rectal wall. During a bowel movement when a rectocele is present, stool typically remains trapped in the bulge. The most significant symptom of a rectocele is chronic constipation or incomplete bowel movements despite fingers inserted into the vagina to assist evacuation, or bridging to assist bowel movement (two fingers shaped like a V pushing up against the labia and/or perineum during defecation). Bowels may still feel full after a movement. Intercourse may be uncomfortable or painful because of pressure of full bowel. Women who’ve been diagnosed with rectocele will gladly share the difficulties they have navigating constipation-it haunts them daily.
Intussusception is the rectum pushing back inside itself (partially inside out), similar to a rubber glove finger pushed into itself when you pull them off. It may appear as finger-like protrusions that branch off of the rectum. Stool becomes trapped in these pockets. An intussusception can be intra-rectal (inside along the rectum), intra-anal (inside along the anus), or extra anal (outside the anus). With the straining that accompanies constipation, these folds sometimes progress and deepen and or reach downward through the anal canal to form rectal prolapse. Common symptoms are chronic constipation, incomplete emptying, pain with bowel movement, blood loss upon defecation, incontinence of gas or feces, or mucus discharge. Upon hard straining, obstructive sensation may increase. Enemas may be ineffective.
Rectal prolapse occurs when rectal walls have prolapsed to the degree they protrude through the anus and are visible outside the anal canal. Patients' with rectal prolapse may experience fecal incontinence. Rectal prolapse sensation may seem similar to an obstacle preventing defecation.
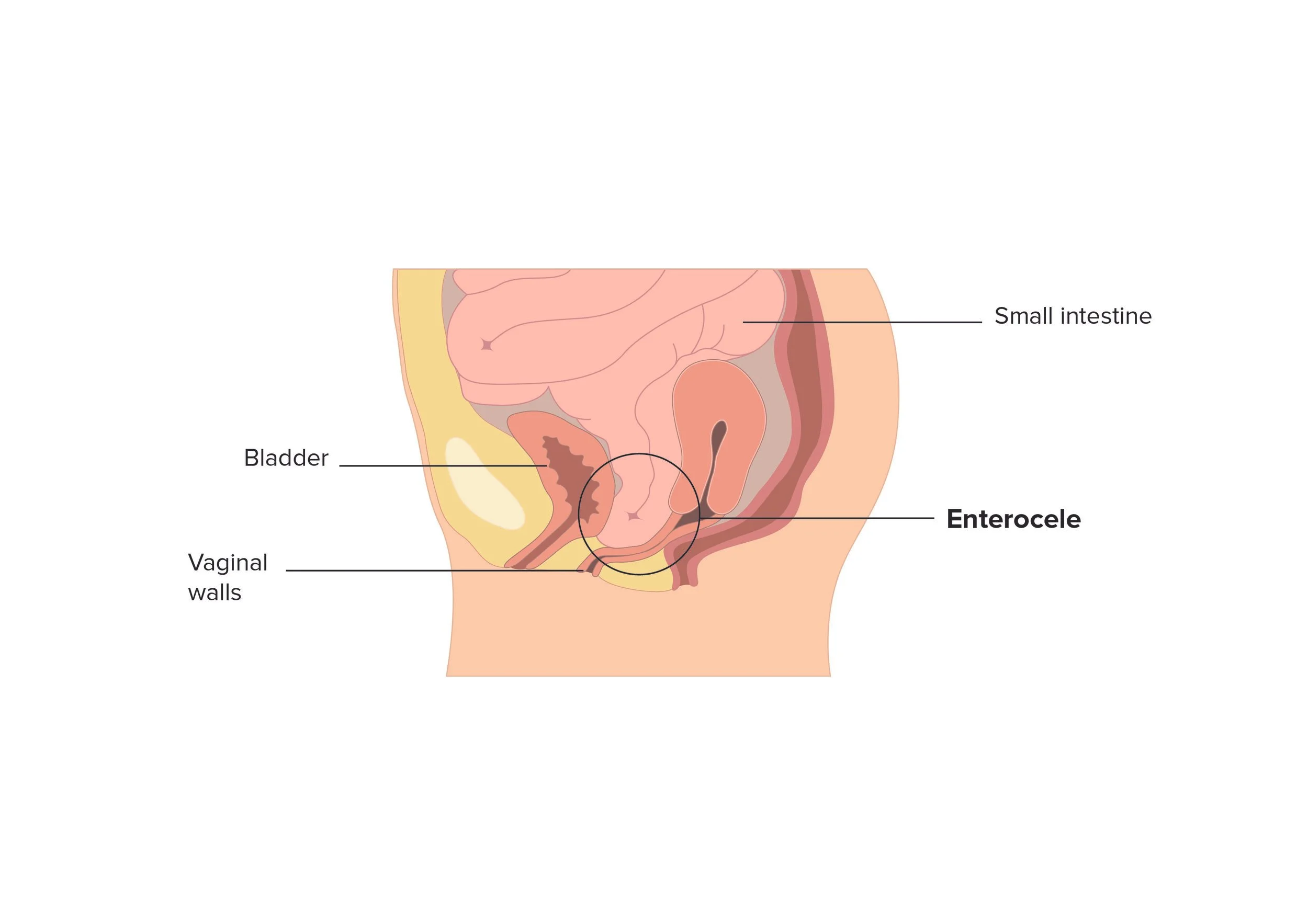
Enterocele occurs when the intestines (small bowel) protrude through a fascial defect or weak tissues, typically at the apex (top) of the vagina. Women who’ve experienced birth trauma or had prolonged deliveries or forceps deliveries may have a higher risk of enterocele. Patients with previous pelvic surgery may have a predisposition to an enterocele as well; particularly a hysterectomy.
An enterocele can develop in the posterior wall (back side by rectum) or anterior wall (front side by uterus), basically wherever the small bowel (intestines) fall through defects in the vaginal wall. The size and “degree of drop” of enteroceles may vary considerably, from halfway down the vaginal length, all the way down to the perineum (tissues surrounding the urogenital and anal openings), or even protrude out of the anal canal to form rectal prolapse. An enterocele may be distinguished during pelvic examination as a bulge that occurs during the valsalva maneuver (deep held breath while bearing down). It may also be necessary for a physician to request you perform the valsalva maneuver while you are standing with one foot on a stool.
Symptoms of an enterocele may be sensation of a mass bulging into the vagina or pushing against the perineum or pain with intercourse. They may also include a pulling sensation in the pelvis or low back pain that eases up when you lie down, vaginal discharge, or a feeling of pelvic fullness, pain, or pressure. There may be a rapid return of bowel movement urge shortly after evacuating bowels (gotta go, gotta go again).
There are 4 types of enterocele:
Pulsion: Caused by continual pressure in abdomen from chronic cough or extreme physical exertion like repetitive heavy lifting.
Traction: Caused by pregnancy, childbirth and estrogen loss which contribute to weakening and stretching of pelvic tissues. Additionally other prolapsed organs may put pressure on tissues contributing to enterocele.
Latorgenic: Cause is not fully known but assumed to be related to hysterectomy or some cystocele repair procedures.
Congenital: Birth defect.
An additional and more definitive diagnostic tool utilized for enterocele is called DRE or defecography (also called proctography). During this test, the act of defecation is assessed by recording expulsion of barium paste that is the consistency of feces. This test can evaluate pelvic floor and rectal function, how well the rectal sphincter works, and the effectiveness of rectal evacuation. Barium is both swallowed (to highlight the intestines) and injected as a paste into the rectum. The patient is sitting on a test commode to mimic normal body language which enables screening of the function of both rectum and pelvic muscle tissue during the procedure. This test facilitates diagnosis of rectocele, enterocele, intussusception, and function of the anal sphincter.
On a more personal note (how much more personal can it get than discussing our bowel concerns, something we ladies do in the APOPS forum almost daily in our individual quest for answers), I’d like to share a few insights. I pay particularly close attention to my body, the signs, symptoms, flags. When something occurs that is the slightest bit left of normal in my pelvic cavity, the wheels are clicking away in my brain, trying to assess whether it is something I need to be concerned about, or share with women navigating POP. My backdrop was transvaginal mesh repair of grade 3 cysto/rectocele; large enterocele discovered during surgery and repaired without mesh. Years ago when I noticed a subtle but palpable loss of sensation front to back as well as a feeling of fullness, I thought to myself, hmmmm, what’s going on in there? Could it be my enterocele is back? Could it be as simple as bloated days related to IBS coupled with scar tissue or adhesions? We all need to recognize that as time keeps ticking away and we move forward with our lives, we must continually monitor change to enjoy continuing quality of life. No one gets a “free health pass” post surgery; we need to remain pro-active.
I do my best to utilize self-awareness along with fitness techniques to address continual shifts in my body. I recognize a distinct difference in how my bowel acts when I eat a healthy low sugar diet with lots of produce, and how it acts when I shove 6 pieces of Dove dark chocolate in my face in one sitting or knock back a few gin cocktails - I’m only human! Every time women with rectal POP issues have a bowel movement, I encourage them to try the following steps to make bowel movements a bit more user-friendly. Lock the bathroom door and "go deaf" to activities and voices outside that door, to assure no one and nothing can disturb you - it will make it easier to relax. And “V-brace” the labia with your first two fingers, pushing against the labia gently, creating some structural support for the pelvic floor, prior to bearing down to have a bowel movement.